Blogue
Chemical Engineers: working in the pandemic’s shadows (Part 1)

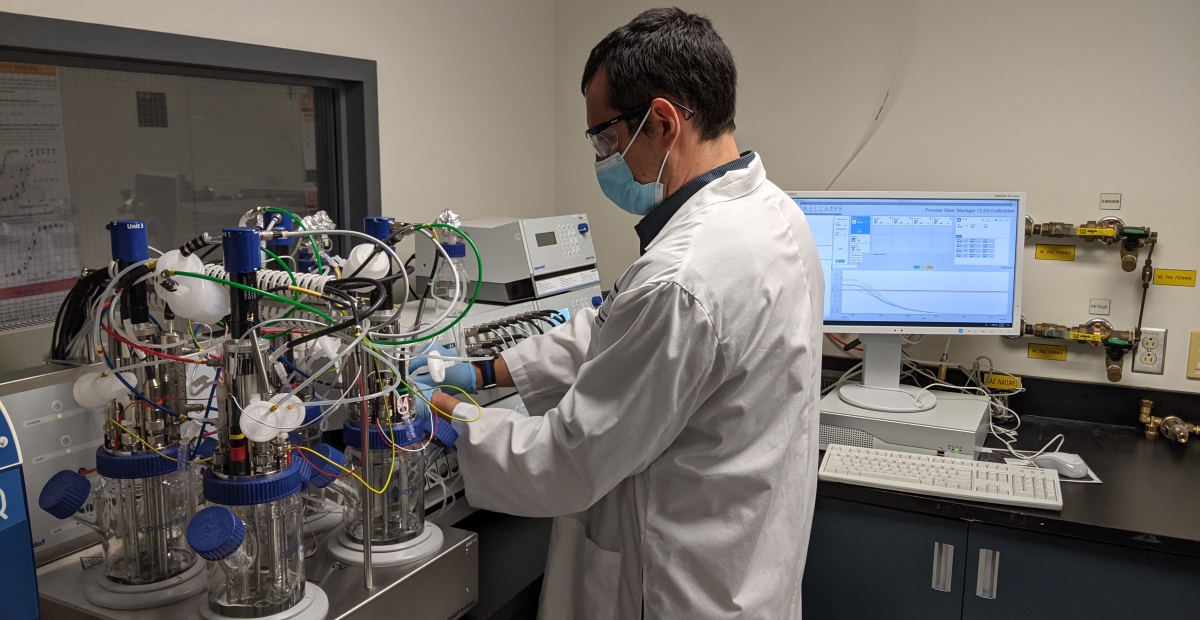
Professor Olivier Henry's brand new bioreactors were quickly put to work to produce billions of copies of the spike protein of the virus that causes COVID-19. (Photo: Martin Primeau)
In the bioreactors in his lab in the J-Armand Bombardier (JAB) pavilion, Professor Olivier Henry's team produces billions of copies of a protein that became famous during the pandemic: SARS-CoV-2's famous “spike” protein - the virus behind COVID-19. This is the first of two blog posts that remind readers of chemical engineers’ important contributions to combat COVID-19.
As the New Year 2020 kicked off, no one could have guessed what the next two years had in store for all of us.
In Wuhan, China, authorities had just reported several cases of fatal, atypical pneumonia. A few days later, the cause was identified: a new type of coronavirus - SARS-CoV-2.
The scientific community sprang into action. On January 10, 2020, the Chinese Center for Disease Control and Prevention had published the virus’ genetic sequence. Pharmaceutical and biotechnology companies all over the world became interested in the problem. Towards the end of the month, German company BioNTech shelved its work on cancer to devote itself entirely to the preparation of an RNA vaccine to slow the outbreak of COVID-19 cases.
Thanks to previously-collected data about other coronaviruses, the protein that will soon become the target of all vaccines is identified: the “Spike” protein. True to its name, this protein allows the virus to attach itself to human cells.
At the end of February, a first case was confirmed in Québec. At the time, the first vaccine candidates were already being tested in various locations – clinical studies were next. At each stage, data was transmitted to health authorities in various jurisdictions.
December 11 2020: approval. The United States’ Food and Drug Administration (FDA) health authority approved use of the vaccine in humans, representing a first for a vaccine against COVID-19, but also a first for RNA-messenger (mRNA) style vaccines.
A glance at... mRna and dna vaccines |
|
The pandemic means that most of us now know what RNA and DNA vaccines are. Yet few know how these two approaches differ from the traditional way vaccines have been made. Instead of injecting protein fragments or complete proteins directly into the host, mRNA and DNA vaccines instead administer a coding sequence that enables cells to produce these proteins on their own. In the case of mRNA and DNA vaccines, this sequence roughly corresponds to a section of the “spike” protein. To produce each of its own proteins, a cell relies on a precise sequence included in the DNA of its nucleus. This sequence is read, then translated into messenger RNA which also contains the information. The latter travels outside the nucleus where a cellular tool called a “ribosome” in turn binds the sequence to make the protein. In the case of DNA vaccines, the process is more complex. To design DNA vaccines, mammalian cells are cultured in a bioreactor which produces adenoviruses, within which is the DNA sequence encoding the "spike" protein. Note that these adenoviruses are harmless and don’t replicate in the body. Once purified and injected into a human arm, they simply pass their DNA on to the host's cells, allowing the host to then make the proteins that will boost their immune system. |
Helping fight the good fight
 Pr Olivier Henry (Photo : Polytechnique Montréal) Pr Olivier Henry (Photo : Polytechnique Montréal) |
In the second part of this Lab 2500 blog post, a Polytechnique Montreal Chemical Engineering graduate - now based in Paris - will tell us how she helped produce thousands of doses of RNA vaccine.
But for the time being, let’s stay in Montréal, and head to the JAB pavilion at Polytechnique Montréal. In his laboratory, chemical engineering professor Olivier Henry had just assembled four small bioreactors each containing up to four liters of cells in culture.
Over the coming months, Professor Henry's team would use these to produce biotherapeutics (biological drugs or biosimilars), or proteins of interest for research purposes.
The bioreactors' first order of business is to produce billions of copies of the “Spike” protein, which will eventually be used in biochemical tests - a project led by a team from the National Research Council of Canada (NRC).
Specialized in bioprocesses, Professor Henry first seeks to optimize the culture conditions of the cells that produce the protein - it's a job that's different each time.
“The challenge for us is to maintain the most homogeneous growing conditions possible," he states. Temperature, pH, rate of oxygen and carbon dioxide in suspension, distribution of cells in the incubator, etc., these are just some of the criteria that must be adjusted to optimize the productivity of cells, but also the preservation of the proteins they make.
"There is know-how, but also a little art," admits the chemical engineering professor, noting that the results sometimes vary for unexplained reasons. Similarity of work is important, since conditions identified on a small scale are, generally speaking, transposed to larger capacity incubators. "Each small gain that we will use to optimize production reduces costs and accelerates production considerably," he adds. It's a strategy is used, for example, to manufacture therapeutic antibodies ... and even viruses serving as vaccines. In fact, in similar - although much larger – bioreactors, DNA vaccines like those produced by AstraZeneca and Johnson & Johnson are made.
Learn more
COVID-19 vaccines mechanism explained (in french)
Pr Olivier Henry expertise
Chemical engineering department website





Comments
Commenter
* champs obligatoire